How AI Gives Patients a Stronger Voice in Healthcare
Among the greatest impacts of AI in patient advocacy is that it allows the patient to be provided with a stronger voice in a healthcare system that may seem overwhelming. Patients who have to address chronic disease, insurance claims, or delays caused by the administration often do not have time, resources, or medical knowledge to express their needs in a constructive manner. This is where AI comes in.
Natural language processing (NLP) tools powered by AI can be used to analyze the feedback emails, online forums, and call transcripts to recognize the issues that are recurring to be addressed. Rather than letting one complaint get lost in a bureaucratic process, AI can combine thousands of voices into patterns that can be identified, pointing to the systemic issues that would otherwise not be noticed. As an illustration, real-time notifications on frequent patient frustrations over a certain insurer refusing to cover certain treatments may be identified to provide advocacy groups with tangible evidence to act on.
In addition to aggregating data, generative AI can be used to enable patients to write appeal letters, insurance claims, or custom health narratives with clarity and precision. Such tools are both time-saving and enhancing the quality of persuasion when communicating with patients. As an example, a patient with cancer who has difficulties when appealing a denied chemotherapy insurance claim may request AI to write a letter with a structure and evidence supporting the claim which references both medical necessity and policy conditions.
AI assistants also contribute to the voice of the patients that has a conversation. Chatbots integrated into advocacy platforms may be used to respond to frequently asked rights-related questions, give advice on the appeals process, and even coach the patients to talk with healthcare administrators. Through the democratization of knowledge access, AI will make sure that no patient becomes voiceless due to the institutional barriers.
The reason why AI is a perfect fit
The distinctive benefits of AI, specifically generative models, machine learning, and natural language processing (NLP) can be applied to address these issues:
- Scalability: AI systems are able to energize numerous additional touchpoints in parallel than one human.
- Speed: The process of automating repetitive tasks makes it quicker in responding.
- Trend identification: AI is capable of identifying trends among the population that would otherwise go unrecognized by individual advocates.
- Personalization: Adapting support to the situation of an individual patient (language, situation, region).
- Closing the gaps: AI-enhanced translation, summarization, or navigation systems can help deal with the problem of literacy or language barriers. Simply put, AI allows patient advocates to accomplish more, faster, and in a more fulfilling manner, and allows human advocates to prioritize deep and high-impact work.
Advantages of AI to Patient Rights and Advocacy
AI serves as an umbrella and a megaphone when it comes to patient rights. Information asymmetry frequently occurs with patients: the insurers, hospitals, and pharmaceutical companies are primarily legal and technical experts, and an ordinary individual cannot compete with them. AI can drive this playing field even.
The first advantage is access to information. Tools powered by AI can be used to translate complicated medical or legal words to simple terms that are easy to understand by patients. An insurance that appeared to be unreadable before can now be divided into simple and doable points. This is not just empowering the patients to get to know of their rights, but it also aids them in making informed decisions within a shorter time.
Fast-tracking of appeals and grievance is also done through AI. Rather than take days or weeks to go through the manual review, AI will be able to produce draft responses immediately, bring out any case precedents, and suggest the next course of action. This will render the appeals process less frightening and more accessible to those who otherwise would surrender.
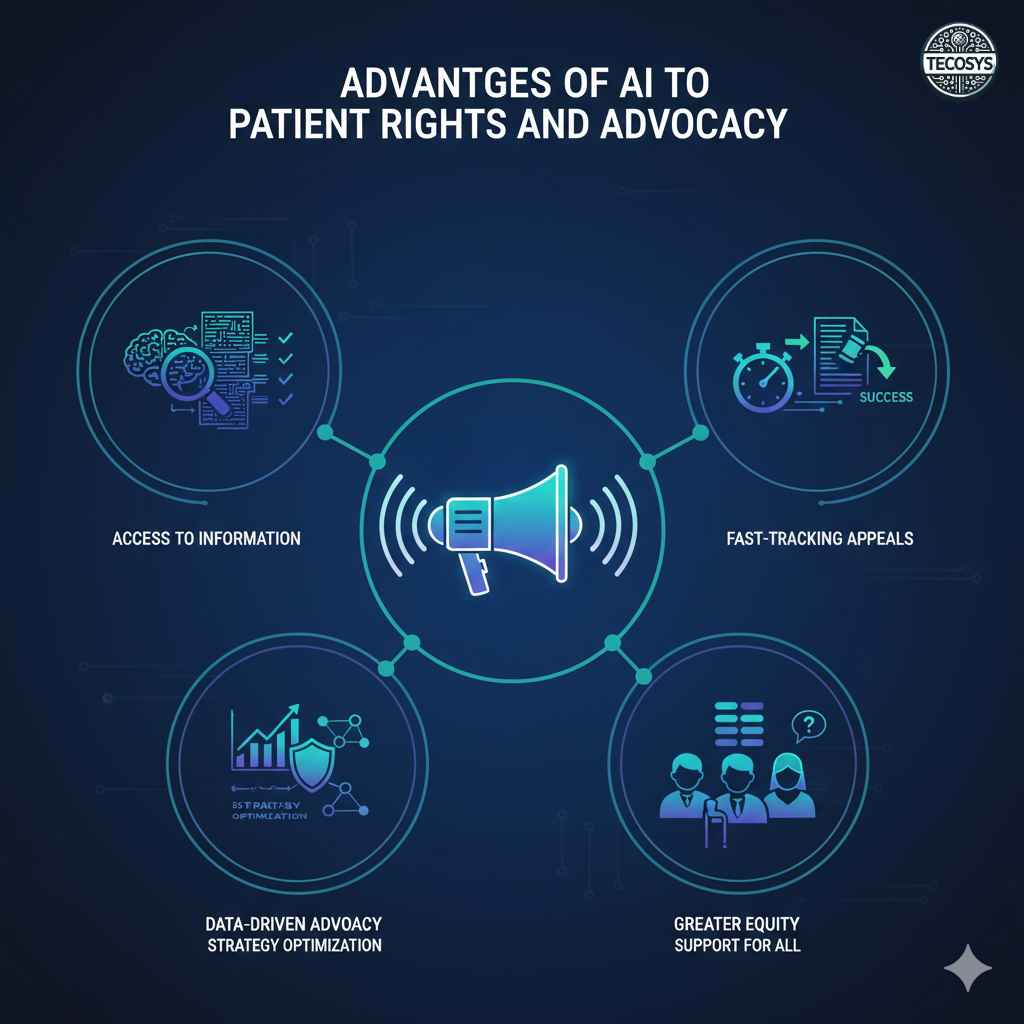
On the part of advocacy groups, AI presents useful information that is data-driven. Through the analysis of case outcomes, denial rates, and success factors, AI can assist organizations in understanding which strategies are the most effective in the context of protecting the rights of patients. This gives them a capacity to distribute the available few resources more effectively and have higher success rates in their advocacy activities.
There is a greater advantage of equity. Even marginalized groups of the population, e.g., rural patients, non-English speakers, and those with low health literacy can be given the same level of advocacy support with the help of AI tools. AI empowers the major concept of equitable healthcare by decreasing access inequality.
Patient Advocacy Group Technology: Roadmap and Best practices
We can map out the path to the responsible and efficient adoption of AI by advocacy organizations (or progressive hospitals).
6.1 Phase 1: Strategy assessment and planning.
- Audit present practices: what is the most time spent by advocates? What are bottlenecks?
- Find out the current AI tools and seek stakeholder feedback.
- Establish success measures (e.g. rate of success on appeals, time saved, patient satisfaction).
- Build governance: assign control, policy, ethical review.
6.2 Phase 2: Pilot & validate
- Begin with modules that are less risky and have a high impact (e.g. drafting letters, summarization, chatbot triage).
- Conduct a pilot of small group, compare results with manual.
- Ensure precision, impartiality, customer contentment.
- Gather qualitative feedback on patients and advocates.
6.3 Phase 3: Scale & integrate
- Progressively increase in complexity (claims appeals, navigation).
- Embark on existing tools (CRM, case management, document systems).
- Train, give instructions and human supervision.
- Watch and watch, often check on bias, mistakes, and drifts.
6.4 Phase 4: Ecosystem & collaboration.
- Collaborate with health systems, health insurers, policy groups, and AI vendors.
- Publicize aggregate (de-identified) data among advocacy groups to increase models.
- Interact with regulators to formulate responsible AI governance.
- Create feedback loops to patients to improve continuously.
Audit present practices: what is the most time spent by advocates? What are bottlenecks? Find out the current AI tools and seek stakeholder feedback. Establish success measures (e.g. rate of success on appeals, time saved, patient satisfaction). Build governance: assign control, policy, ethical review.
Artificial Intelligence Healthcare Navigation
The journey through healthcare has been termed as one of the most stressful to go through by the patients. Among the decisions on providers, appointments, and referrals, and the insurance, most patients are confused even before they receive treatment. This is the solution of AI-driven healthcare navigation.
AI may assess the insurance plan of a patient, his or her medical history, and geographical location to suggest the most affordable and quality providers with whom he or she is covered. The patients will not have to browse the directories manually, instead, they will be given customized recommendations, like: Here are three in-network cardiologists within 20 miles of you, with the shortest wait times and the highest quality rating.
In addition to the use of AI in the selection of providers, it can also help with appointments. Intelligent systems will be able to arrange availability among doctors, specialists and centers of diagnosis to cut down delays which usually extend the care. They also have the capability of flagging the need to pre-authorize and even automate some of the approval process.
Navigation is also spread to financial clarity. AI-based tools can also approximate out-of-pocket costs, find the lowest costs of treatment in different providers and alert patients about the possible presence of unexpected bills. Such transparency is vital in a nation where the medical debt has been a contributing factor to financial distress. Lastly, AI guarantees constant trip monitoring. In case a follow-up test is not booked or a claim denial is received by the system, AI systems can send a reminder to patients and advocates. This is a way of avoiding the slip up of the important steps which would otherwise fall between the cracks thus enabling the patient to gain the timely care.
Introducing AI to Reduce Healthcare barriers
Although the advocacy has long concentrated on personal struggles, AI enables the focus on systemic access to care. Language and literacy are one of the greatest impediments. A lot of patients have little or no ability to comprehend medical jargon or they do not speak English as a mother tongue. Translation and simplification tools powered by AI will make sure that instructions, forms, as well as educational materials are provided to everybody, irrespective of their background. Geography is the other barrier. Patients that are rural or underserved usually do not have access to advocacy groups or experts.
Time and resource challenges are also addressed using AI. Smaller advocacy groups may apply AI to address the simple questions, prepare standard letters, and conduct case intake. This enables human advocates to commit their efforts to intricate or high-red cases in which empathy and negotiation talents are the most required.

Noteworthy, AI is able to identify vulnerable patients who may be challenged. Practically an example is, predictive algorithms can detect those patients that are most likely to miss a follow-up because of a transport problem, because of financial strain, or because of poor literacy.
Through such an understanding, the advocates can intervene in advance before issues snowball. With these barriers systematically minimized, AI not only enhances personal experiences but also reflects positively on the health outcomes of the population due to the promotion of greater access to quality and timely care.
Technology for Patient Advocacy Groups
To advocacy organizations, AI is not merely a useful tool anymore but is turning out to be a strategic requirement. These units are usually overwhelmed with too many cases, small budgets and pressured to achieve immediate outcomes. AI offers several solutions. To begin with, AI is helpful in workflow efficiency. AI-based case management systems are capable of arranging the patient records automatically, tracing the case progress, and focusing on urgent matters. Rather than manually going through files, advocates are able to be directly involved in solving a problem.
Second, AI presents information intelligence. Advocacy groups are able to compare their patterns across cases and point to systemic issues, such as when a specific insurance company consistently refuses certain treatments. These understandings enable groups to lobby on changes in policies using evidence at heart.
Third, AI improves a large-scale communication. Organizations have the ability to respond to the queries that are often asked by patients 24/7 with chatbots and automated response systems, even without having more staff. This does not substitute human advocates, but enhances their scope to a great extent.
Fourth, AI is the power of collaboration. Advocacy groups can also come up with more powerful frameworks and exchange best practices by exchanging anonymized data between networks. This forms a concerted effort to counter systemic challenges, which makes them that much more effective.
The artificially intelligent is transforming the advocacy of patients. The potential is enormous in terms of providing patients a more powerful voice, facilitating the process, decreasing systemic barriers, and providing advocacy groups with more intelligent tools. However, technology will not bring the success by itself. To make sure that AI not only does not harm but also enhances trust in healthcare, it will be necessary to deploy it ethically, to be transparent, to have patients consent, and to control humans.
At Tecosys, we are sure in using the latest technology and human kindness to create a future in which all patients are listened, assisted, and cared. AI will not come to disenfranchise advocates but will empower them to reach more people in need. Smarter, fairer and more compassionate patient advocacy is the future and AI is the engine that can accomplish that revolution.
Frequently Asked Questions
Q1. Will patient advocates be substituted by AI?
No. AI is not a replacement, but a complement. It takes minor cases, whereas human champions are concerned with complicated, sympathetic cases.
Q2. Why does AI safeguard patient rights?
To empower patients to exercise their rights, AI assists in translating complex policies and draft appeals and analyzing systemic patterns of denial.
Q3. Are small advocacy groups able to afford AI?
Yes. A large number of AI tools are scalable and cloud-based, and can be used by smaller organizations on a subscription or shared basis.
Q4. What is the role of AI in medical care barriers?
With the offering of multilingual support, remote assistance, predictive insights to at-
risk patients, and time-consuming processes automation.
Q5. What are the ethical issues of AI-powered advocacy?
Among the concerns are privacy, bias, and transparency. They should be dealt with by strong protection, human control, and open disclosure to patients.
Want AI that empowers patients while keeping their data safe?
Discover how Tecosys AI Solutions can transform the way you support patients — smarter navigation, stronger rights, and trusted care.
Book a demo today and see why Tecosys is the future of secure, ethical, AI-powered patient advocacy.
📧 Email: [email protected]
🌐 Visit: www.tecosys.in